Major Reasons DNP Projects Are Rejected
We spoke to more than 20 practicing professors and they gave 15 major reasons why DNP projects are rejected. We’re here to make sure all the months of painstaking research plus those long nights drafting the DNP capstone project paper aren’t in vain! This article purposes to help DNP finalists identify, understand, and overcome the most frequent reasons why their DNP project may be rejected.
Every single DNP student dreams of seeing their project approved on the first submission. Yet, nearly 49% of all DNP capstone project papers in 2025 were outrightly rejected or sent back for revisions. Most of these failures stem not from a lack of student effort but from avoidable design, compliance, or documentation errors.
Tease your lecturer with confident academic communication and pristine structure using our proven strategies that improve success rates. Talk to our expert DNP project writers NOW!
DNP Capstone Projects Demonstrate Scholarly Clinical Aptitudes, Nursing Leadership, and Evidence-Based Practices
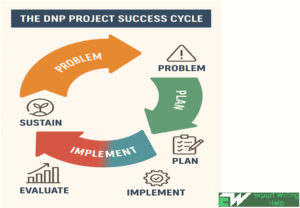
DNP capstone papers wrap scholarly experiences for graduates by demonstrating advanced clinical scholarship traits, nurse leadership competencies, and EBP to address real-world healthcare challenges. Although heavy criticism and substantial project redesigns are common in a DNP journey, nobody wishes for a stalled project, total rejection, or program withdrawal in extreme cases.
The rising number of modern DNP programs has pushed some institutions to develop specific Project Ethical Review Committees (PERCs) that manage the sheer volume and academic rigor of DNP capstone submissions. This decision is informed by 87% of faculty today being somewhat or very dissatisfied with the papers they receive. A whooping 64.5% of DNP students don’t have time to write a quality capstone project paper, while 63.8% of those we interviewed had difficulty knowing how to even get started. Official statistics on outright withdrawal from nursing programs aren’t published yet.
Need help with writing a DNP capstone paper to avoid rejection or forceful program withdrawal? Place your order with us TODAY for A+ grades. Click here.
What Makes a Successful DNP Capstone Project Paper?
You’re probably wondering how our team of experts assists DNP students the world over to write custom capstone project papers that earn high grades all the time. Simple – we follow the following guidelines strictly for each order. Feel free to share this 10-point guide with the 2025 cohort so that everyone in your class graduates with high marks:
- Our inhouse practicing expert writers are DNP graduates with years of experience on their sleeves. These gurus know the difference between traditional research and DNP capstone projects. If you couple that with an A-list of distinguished consultants in all the 14+ nursing disciplines and English language grandmasters, you get a winning DNP capstone paper every time!
- From the assessment brief and your specific assignment instructions when placing an order, we deliberately focus on applying classroom knowledge to real-world nursing scenarios to improve your practice
- Nobody knows institutional requirements including IRB approvals, sustainability plans, and organizational support better than us!
- We match every single order to AACN essentials, clearly discuss measurable research outcomes, and succinctly present evidence-based changes
- We don’t take your DNP capstone project as just another academic activity or draw a topic from a generalized area of nursing interest. We guarantee you a sharp, personalized, problem-focused, and data-backed paper that addresses a significant gap in contemporary nursing practice
- Every DNP project paper we send to your inbox impacts outcomes at a systems level (micro-, meso-, or at the macro-level) or for a specific population. Ours is a platform for future scholarly practice with SMART objectives and outcomes
- Your DNP project report positively contributes to the vast body of scholarly knowledge in nursing practice. There’s a concrete plan on sustaining changes within the organization after your involvement ends in consideration of financial, systems, and political realities
- The project findings are shareable beyond academic settings through oral or poster presentations at professional conferences. Yes, you can submit our final manuscript for publication in a peer-reviewed nursing journal!
- A feasible and realistic DNP project timeline with a detailed description of data collection / analysis methods, project design, setting, and samples
- A winning DNP capstone project paper with zero AI-generated phrases, which doesn’t plagiarize authoritative nursing literature, and finely combed for English grammar errors
15 Major Reasons DNP Projects Are Rejected — And How You Can Overcome Them
Let’s take a look at 15 of the major reasons why your DNP project could bounce and how to fix them. Also included are practical examples and best practice tips from our DNP capstone project submission archives. I’ve split the weaknesses into 3 major categories (conceptual and topic-related issues, design / methodological weaknesses, and ethical, institutional & formatting errors):
| # | Reason for Rejection | How to Avoid / Fix | Best Practice Tip / Example |
| Category A: Conceptual and Topic-Related Issues | |||
| 1 | Weak (vague) statement of the problem
Many DNP project proposals fail because their thesis statement is either too broad or lacks measurable focus. A DNP project review committee wants clarity on the “why” and “how” of your capstone project |
● Use a PICOT question to define the research population, possible interventions, comparisons, projected outcomes, and a feasible timeframe
● Write a concise, evidence-supported problem statement linked to a measurable impact |
Replace the ambiguous “How to improve patient outcomes for rural populations,” you could sharply focus the DNP research question to “Reducing catheter-associated infections for rural ICU patients through nurse-led hygiene protocols” |
| 2 | The research topic is too broad or too narrow
A DNP project that covers too much ground is unmanageable. An overly narrow research topic lacks measurable impact
|
● Narrow the focus to a manageable, high-impact issue
● Use PICO or PICOT to structure the research topic ● Get DNP topic selection assistance from a human agent 24/7/365 |
Instead of a bland “Improving patient safety,” you may focus on “Reducing medication errors in post-op patients” |
| 3 | Research doesn’t match with the DNP scope or competencies
– Your project will fail if it doesn’t clearly demonstrate the application of advanced nursing practice, leadership, or evidence-based improvements in healthcare
– If the clinical or organizational problem isn’t clearly defined (or lacks significance to patient outcomes and overall health system performance), you will surely fail
|
● Ensure your DNP capstone project addresses clinical practice improvements, leadership, or patient outcomes as defined in the AACN DNP Essentials (2021) | Synchronize your research objectives with AACN Essentials 2021 (for example, systems thinking and interprofessional collaboration) |
| 4 | Unclear linkage to evidence-based practice (EBP)
A DNP proposal that lacks a strong foundation in current research, guidelines, or best practices is bound to fail |
● Conduct a thorough literature review from the past 5 years
● Cite authoritative, peer-reviewed EBP sources |
Integrate at least 13 relevant, recent studies in your submission that justifies your intervention or the QI approach |
| 5 | Misalignment between the research problem, purpose, and objectives
The DNP project’s purpose or aims should logically flow from the identified problem and lead the audience to conceptual inconsistencies |
Ensure a logical flow: Problem → Purpose → SMART Objectives → Outcomes | If your problem is on poor hand hygiene for example, your purpose should focus on improving compliance through public sensitization programs, NOT general infection control |
| Category B: Methodological and Design Weaknesses | |||
| 6 | Inappropriate (poorly justified) project designs
Using the wrong approach (e.g., research instead of quality improvement) or not explaining why the chosen design fits the problem amounts to rejection
|
Match your DNP project design to the purpose of study (e.g. QI, process improvement, program evaluation) and justify why it’s most appropriate | Use Plan-Do-Study-Act (PDSA) for quality improvement or a logic model for implementation |
| 7 | Inadequate data collection and/or analysis plan
Many DNP project reports miss critical details on how data will be gathered, analyzed, or interpreted. Watch out for pre- and post-intervention comparisons
|
Describe in detail your data sources, analysis tools, timelines, and analytical methods | Use validated data collection and analysis tools such as the Maslach Burnout Inventory or Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) |
| 8 | No measurable outcomes and the conspicuous absence of evaluation metrics
DNP projects are rejected whenever their success can’t be quantified through valid, reliable indicators.
|
● Define clear, quantifiable indicators (clinical, process, and satisfaction outcomes)
● Make a list of SMART goals at early stages of the project report |
An example of a SMART goal would be “To increase fall risk assessment compliance from 60% to 90% within eight weeks” |
| 9 | Zero planning on sustainability and project implementation within the report
Nursing capstone projects that fail to describe how improvements will be maintained after the intervention period definitely earn a rejection
|
Add a post-project plan showing how you will maintain improvements; for example through staff training or policy integration | We always include a sustainability / implementation plan tied to annual performance reviews or the QI dashboard for every DNP capstone project order |
| 10 | Insufficient stakeholder engagement
Not involving key stakeholders like nursing leaders, clinicians, and patients weaken feasibility and organizational buy-in. It is also a direct ticket for your DNP project to be rejected
|
Involve key leaders early in your project. Include the feedback of nurse managers, physicians, and QI committees | Create an analysis matrix that shows the roles, interests, and support levels for every stakeholder |
| Category C: Institutional, Ethical, and Formatting Errors | |||
| 11 | Missing organizational approval or a supporting letter
Most nursing schools require a letter from the practice site to confirm partnership and feasibility
|
Obtain a formal site approval or attach a partnership letter confirming feasibility and data access for your DNP project | Attach a signed, certified letter from the Chief Nursing Officer or site director |
| 12 | Failure to obtain IRB or ethical clearance
Proposals that skip ethics approval, especially when involving patient data, are immediately disqualified
|
● Secure an IRB / exemption approval before implementing your project
● Include relevant documentation in the appendices |
Mention for example “IRB APPROVAL RECEIVED FROM XXX UNIVERSITY, PROTOCOL #003 of 2025” or its equivalent, and annex supporting documents |
| 13 | Plagiarism, using GPT and AI writing tools, or weak academic integrity
Projects containing copy-pasted texts, improperly cited evidence, or in violation of institutional policies on GPT and the use of AI tools are immediately rejected
|
● Before submission, run your assignment through plagiarism and AI-detection tools like Turnitin, GPTZero, CopyLeaks, or Grammarly Premium
● Cite every source correctly using APA (7th edition)
Did You Know?
You can book for cheap AI text humanizing services and help with referencing! |
● If you can’t write 100% organic content like our experts, paraphrase ideas instead of copying text
● Maintain a 5% or less similarity index ● Ensure your submission has less than 20% flagging for AI content (considered as the maximum limit for false positives) |
| 14 | Incomplete or non-compliant submission
Missing whole sections like an abstract, logic model, evaluation plan, or incorrect formatting as per the DNP manual guidelines lead to rejection
|
● Strictly adhere to your institution’s DNP manual and the assignment brief
● Check that your final draft has a title, an abstract, a logic model, evaluation tools, and appropriate appendices |
Download a free DNP Project Checklist before submission to ascertain all mandatory sections are present |
| 15 | Poor writing quality with no scholarly tone
Unclear, disorganized, and non-academic writing tone undermines the credibility and readability of a DNP capstone paper, resulting to rejection
|
● Write in clear, logical, academic, and evidence-based language
● Follow specific DNP formatting guidelines preferred by your faculty ● Adhere to a single referencing technique ● Let your research flow in a logical, error-free style |
Use the third-person, objective tone: for example, write “The findings indicate that…” but not “I found that…” |
Subscribe to Our Affordable DNP Capstone Project Help Service Today!
The 5 strategies below always delivered a strong DNP project proposal for our clients:
- Ground your project in AACN DNP Essentials (2021). Review ethical and institutional compliance guidelines before you start
- Use PICO / PICOT and SMART objectives for precision
- Maintain strong stakeholder engagement from planning through to project evaluation
- Include clear evaluation metrics. Discuss favorable sustainability and dissemination plans
- Seek the opinion of mentors or qualified others. Ask a qualified person to help with thorough proofreading and formatting reviews before submission
DNP Students Also Ask
Qn: Do all DNP projects need IRB approval?
Ans: No. Only DNP projects involving human participants or data from human participants require IRB reviews or institutional determination.
Qn: What’s the prime difference between a quality improvement project, a research study, and EBP in DNP?
Ans: QI uses systematic processes to improve patient outcomes whereas a research study applies quantitative or qualitative methodologies to develop new knowledge. EBP seeks and applies the best clinical evidence, often from research, towards making sustainable patient-care decisions.
Qn: How long does a DNP capstone project take from start to approval?
Ans: A DNP project takes 18 to 24 months from start to final approval. The exact duration depends on whether you’re enrolled full-time or part-time, the intricacy of the project, and approval process efficiencies at your institution or clinical site.

 Nurses can attain excellent outcomes for their patients through evidence-based practice, however, they often don’t share their experiences with fellow nurses in their own or other healthcare facilities. This leads to pointless replication of efforts and propagates clinical approaches that aren’t evidence-based.
Nurses can attain excellent outcomes for their patients through evidence-based practice, however, they often don’t share their experiences with fellow nurses in their own or other healthcare facilities. This leads to pointless replication of efforts and propagates clinical approaches that aren’t evidence-based.
 Earning a master’s degree in nursing is not the end of your academic career. Yet, there are occasions when going forward seems like an impossible task. Maybe you’ve hit a wall and aren’t sure what to do next. In fact, this occurs frequently.
Earning a master’s degree in nursing is not the end of your academic career. Yet, there are occasions when going forward seems like an impossible task. Maybe you’ve hit a wall and aren’t sure what to do next. In fact, this occurs frequently.
 Committing to ongoing learning and education improvement is a requirement for success in the healthcare sector. There are many opportunities for advancement in nursing; the trick is to determine which ones are best for you. Because of this, nurses at all levels are looking for ways to advance in their careers and are trying to figure out what degree will help them land the jobs they want. This typically entails earning a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). Some also might think earning a Bachelor of Science in Nursing (BSN) is the best choice.
Committing to ongoing learning and education improvement is a requirement for success in the healthcare sector. There are many opportunities for advancement in nursing; the trick is to determine which ones are best for you. Because of this, nurses at all levels are looking for ways to advance in their careers and are trying to figure out what degree will help them land the jobs they want. This typically entails earning a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). Some also might think earning a Bachelor of Science in Nursing (BSN) is the best choice.